Education Changes Tomorrow, Stay Away from Rumors and Fight Sugar Together
1. Diagnosis and classification of elderly diabetes mellitus
l The diagnostic criteria, clinical classification (no gestational diabetes) and tertiary prevention of diabetes in elderly patients were the same as those in young and middle-aged patients.
l Normal fasting blood glucose, postprandial hyperglycemia and insulin resistance are the characteristics of newly diagnosed elderly diabetic patients.
l Diabetes screening should be included as a routine item in the annual physical examination of the elderly. Fasting blood glucose should be combined with blood glucose or glycosylated hemoglobin (HbA1c) 2 hours after loading, which is conducive to reducing missed diagnosis in a single examination.
l The diagnostic criteria of HbA1c in elderly patients with diabetes mellitus were <6.0% in normal subjects. Impaired glucose regulation (IFG, IGT, IFG+IGT) 6.0-<6.5%; Diabetes ≥6.5%.
2. Blood glucose monitoring methods
The most basic monitoring point
|
Morning, before dinner
|
The most commonly used monitoring site
|
Three meals before dinner + evening before bed
|
Optional monitoring points
|
Before breakfast + 2 hours after meals
|
The most comprehensive monitoring site
|
Three meals before meals + 2 hours after meals + evening before bed
|
Add points if necessary
|
2-3 a.m., or special needs |
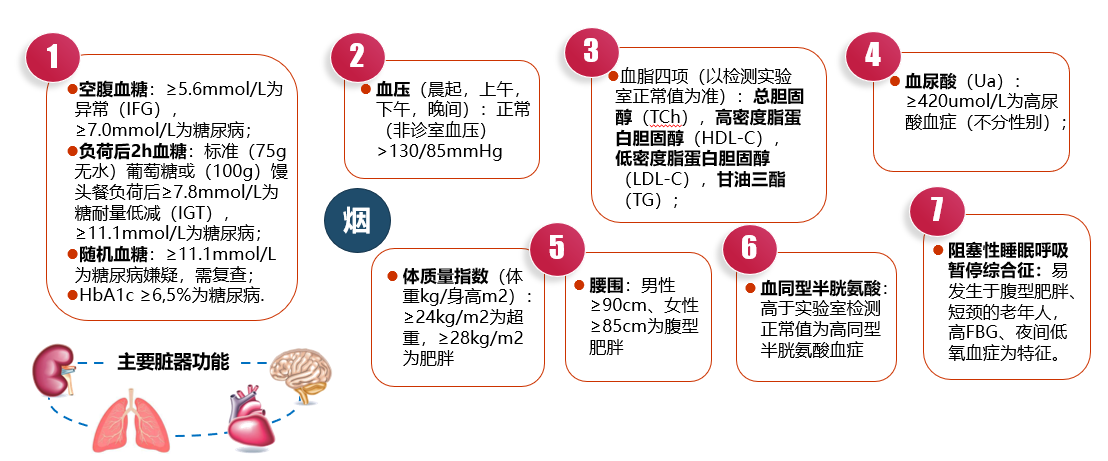
Iii. Assessment of metabolic risk factors associated with cardiovascular disease
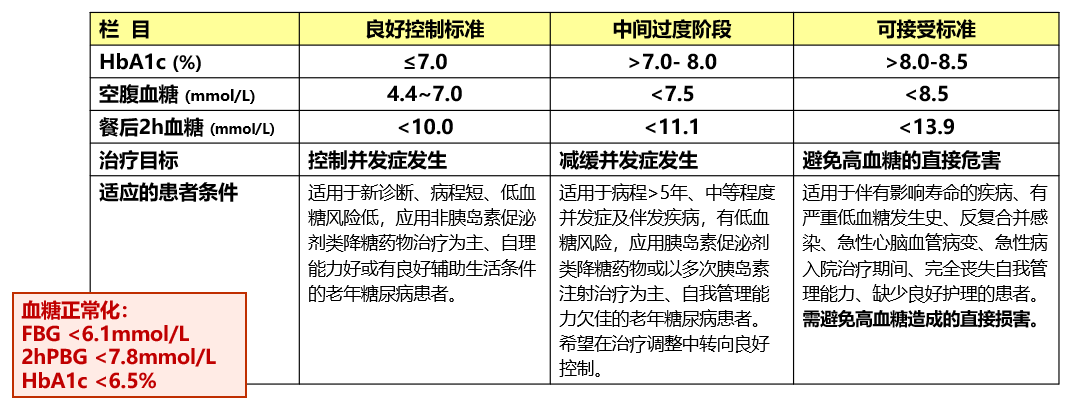
Fourth, elderly diabetes blood sugar control: personalized calibration, and strive for the best
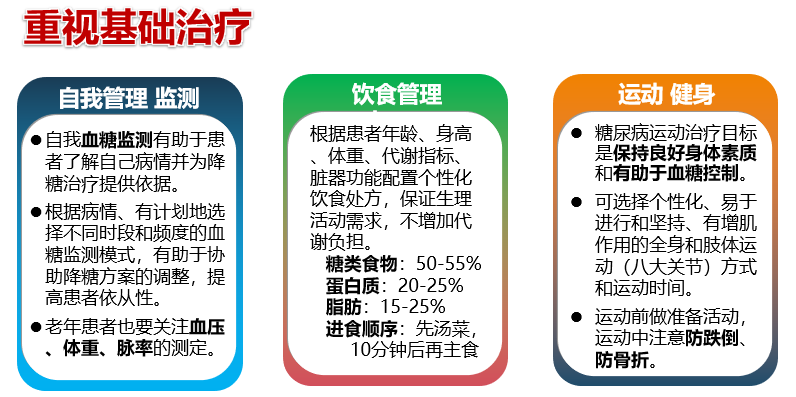
Five elderly diabetes treatment
 Individual formulation of hypoglycemic program
Individual formulation of hypoglycemic program
l Metformin is the drug of choice (no age limit) and can be used for a long time (except for renal insufficiency).
l On the basis of lifestyle management and metformin treatment, HbA1c was higher than 7.5%, and earlier combined treatment had better effect on overall blood glucose control.
l SGLT-2i or GLP-1RA is preferred for patients with atherosclatherosclastic cardiovascular disease (ASCVD) or high risk factors, kidney disease or heart failure.
l After lifestyle and oral hypoglycemic drug treatment, the blood sugar still fails to reach the control goal, insulin therapy should be started, and basic insulin is the first choice.
l Multiple insulin injections (intensive therapy) or continuous subcutaneous insulin infusion (CSII) are recommended for patients with hyperglycemia (HbA1c >9.5%, FPG>12mmol/L), infection or acute complications, surgery or stress. Reassessment and adjustment after remission.
Six, "early prevention, early diagnosis, early treatment, early standards", high quality of elderly life
l Long-term poor blood sugar control is the direct cause of diabetes complications.
l Elderly diabetic patients should control their blood sugar within the acceptable range as far as possible to avoid hyperosmatic coma or ketoacidosis and other acute complications.
l Elderly diabetic macrovascular disease is jointly affected by other cardiovascular disease (CVD) pathogenic factors, the damage to the heart, brain and kidney function is more serious, need to pay attention to, regularly assess the risk, and strive to plan for a rainy day.
l Diabetic neuropathy and diabetic nephropathy are often affected by non-diabetic factors in elderly diabetic patients, so it is necessary to be vigilant and formulate overall prevention and control measures.
l Early screening and treatment of diabetic retinopathy and diabetic foot disease have positive effect on improving prognosis.
l Through self-management and blood glucose monitoring, active and stable control of blood glucose for a long time is expected to reduce the occurrence of diabetes complications.
Endocrine metabolism branch contribution
(The opinions expressed are solely those of the author. Some pictures in this article are from the Internet, if there is infringement, please contact to delete)

