How much do you know about chest pain ultrasound in the elderly
"What's wrong with you, old man?" "Doctor, I have a pain in my chest." "What kind of pain? A stuffy pain? Tearing pain..." This is a conversation a lot of doctors have with patients in the emergency room. Chest pain is a common symptom of many diseases, especially cardiovascular disease, and sometimes it is difficult for clinicians to make a clear diagnosis based on symptoms, which requires ultrasound (mainly including echocardiography, vascular ultrasound, etc.). Ultrasonic examination is the eye of clinicians, and it is widely used in clinical diagnosis of multi-organs with the advantages of non-invasive, non-radiation, real-time and convenient, which provides valuable information for clinicians and plays a vital role in the differential diagnosis and timely treatment of diseases. Common elderly patients with chest pain that require ultrasound are as follows:
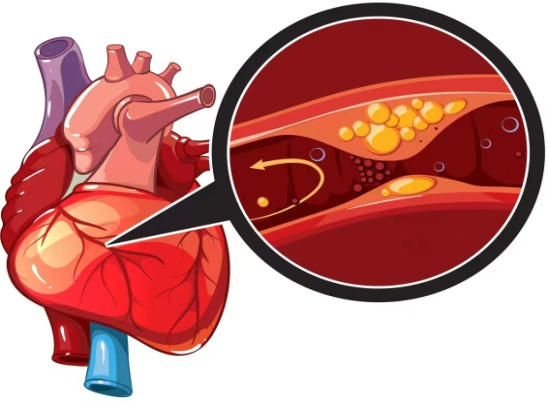
 1. Acute myocardial infarction
1. Acute myocardial infarction
Chest pain is similar to angina pectoris, persistent intense pain in the retrosternal or precardiac area, lasting more than 30 minutes and not relieved by rest or nitroglycerin. However, some elderly people, diabetes and other patients have atypical symptoms. Acute heart infarction (AMI) is caused by coronary atherosclerotic plaque bleeding, avulsion, thrombosis and other reasons, leading to lumen occlusion, blood flow interruption, and acute myocardial ischemia and necrosis in the blood supply area. Echocardiography indirectly determines the state of blood supply to the heart muscle by observing the ability of the ventricular wall to diastolic and contractile movements. The characteristic manifestations of coronary heart disease are the reduction, loss and contradictory movement of cardiac wall or the decrease, non-thickening or thinning of cardiac wall during systolic period. The diagnosis of acute and chronic myocardial infarction is based on local ventricular wall thinning, loss of motion or contradictory motion, and decreased or enhanced myocardial echo. Combined with electrocardiogram examination, it provides strong support for clinicians to improve indirect imaging evidence and whether to perform digital subtraction angiography.
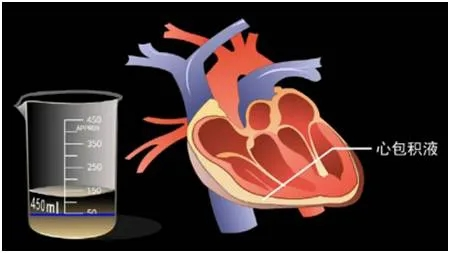
 2. Acute pericarditis
2. Acute pericarditis
Pain or dull pain in the precordial area, most of which are different in nature from angina, can be sharp pain, dull pain or crushing pain. The pericardium may cause acute reactions and chronic diseases such as pericardium adhesion and constriction due to bacterial, viral, autoimmune, physical, chemical and other factors. Echocardiography is of great help in the diagnosis of pericardial diseases, especially pericardial effusion, and the diagnostic accuracy is very high. The liquid dark area between the visceral layer and the parietal layer of the pericardium can be seen in the examination, and the abnormal reflection can be seen in the liquid dark area of the systolic period during the examination of the apex of the heart. In addition, echocardiography plays an irreplaceable role in determining the backlog of pericardial effusion, selecting the puncture site and guiding pericardial puncture operation, and space-occupying lesions in pericardial cavity.
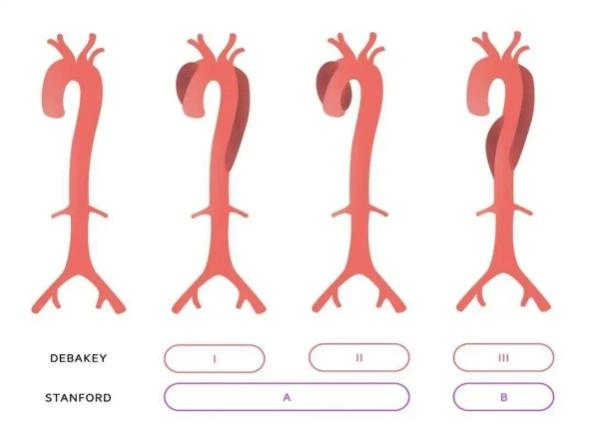
3. Aortic dissection
The chest pain is severe and continuous, with tearing and knife-cutting sharp pain, and there are a few patients with chest pain symptoms are not obvious, only manifested as chest discomfort. Hypertension is the most common cause of the disease. The aorta is the main artery of the systemic circulation and the largest artery in the whole body. It is issued from the left ventricle of the heart, slightly arcuate upward to the right and downward, and then downward along the spine. According to the walking and position of the aorta, it can be divided into three sections: ascending aorta (ascending aorta), aortic arch and descending aorta (descending aorta), of which the descending aorta is bounded by the aortic hiatal hole of the diaphragm. It is divided into the thoracic aorta (aortic chest) and the abdominal aorta (aortic abdomen). Transthoracic echocardiography has special advantages in its diagnosis. Multiple sections can show the widening of the ascending aorta and the tearing of its intima, which divides the aorta into true lumen and false lumen, and there may be different degrees of thrombosis in the false lumen. In the section of the superior sternal fossa, endodenudation of the ascending aorta, aortic arch and descending aorta can be observed, showing linear or cord echo. It pulsates and has a floating sensation. Aortic dissection can compress the relevant branches of the aorta, resulting in vascular stenosis and occlusion, so it is generally combined with vascular ultrasound examination. Transesophageal echocardiography makes up for the shortcomings of transthoracic echocardiography in unclear display of descending aortic arch and incomplete exposure of thoracic aortic segment. It can clearly show the entire aorta, clarify the scope and degree of endarterectomy, the location and size of the break, and distinguish between true and false lumen, etc., and can be classified for diagnosis. However, in cases of critical illness, irritability or inability to work together, transesophageal echocardiography can be used for classification. Special attention should be paid to careful selection to avoid accidents.
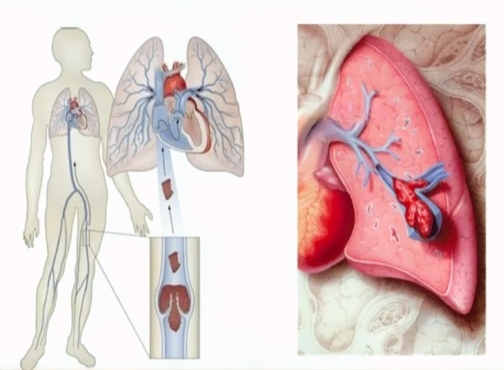
 4. Acute pulmonary embolism
4. Acute pulmonary embolism
Difficulty breathing, chest pain. It is currently one of the leading causes of death in many Western countries. Echocardiography is an important part of the imaging diagnosis. The direct sign is the discovery of embolic echo in the main pulmonary artery and left and right pulmonary artery branches, and the indirect sign is the enlargement of the right heart. Widening of pulmonary artery. Abnormal ventricular septal movement, tricuspid regurgitation, pulmonary hypertension and other pulmonary circulatory disorders. Deep vein thrombosis is the main factor leading to pulmonary embolism. Embolic emboli can come from the upper and lower vena cava system or the right heart, mostly from the deep veins of lower limbs. Therefore, the real culprit of pulmonary embolism should be identified by ultrasonography of lower limb veins and plasma D-dimer for diagnosis. Diagnosis depends on radionuclide lung scan or pulmonary angiography.
When you have the symptoms of chest pain, do not be lucky, must be timely medical treatment, according to the need to check, symptomatic treatment, health often with you and me.
Author: Department of Ultrasound Medicine, Beijing Fengtai Teaching Hospital, Capital Medical University
Contributor: Song Ye and Wu Dongfang
(The opinions expressed are solely those of the author. Some pictures in this article are from the Internet, if there is infringement, please contact to delete)

