[Micro Popular Science] Bone Marker Screening, Early Warning of Osteoporosis
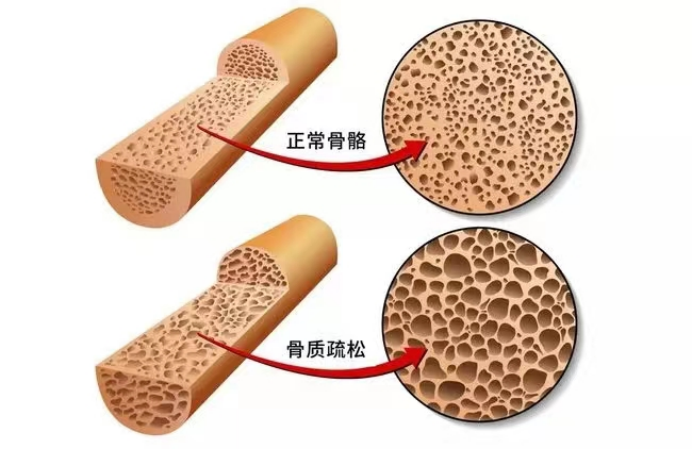
What is Osteoporosis?
Osteoporosis is a systemic bone disease characterized by low bone mass, microstructure damage of bone tissue, increased bone fragility, and easy fracture. Osteoporosis usually does not have obvious clinical manifestations in the early stage, if not paid attention to, as the disease progresses, patients will have bone pain, spinal deformation, and even brittle fractures, disabling and fatal consequences.
What are the risk factors of osteoporosis?
1. Uncontrollable factors
Race, aging, female menopause, family history of fragility fracture, etc.
2. Controllable factors
1) Unhealthy lifestyle: low physical activity, insufficient sun exposure, smoking, excessive alcohol consumption, calcium and/or vitamin D deficiency, etc.
2) Disease impact: including diabetes, hyperthyroidism and other endocrine system diseases, rheumatic immune diseases, gastrointestinal diseases, blood system diseases, chronic liver and kidney diseases.
3) Drug effects: including glucocorticoids, proton pump inhibitors, antiepileptic drugs, aromatase inhibitors, gonadotropin releasing hormone analogues, antiviral drugs, etc.

Who needs to test for bone markers?
? Women over 50 and men over 65 with unexplained chronic low back pain
? Women after natural menopause or bilateral oophorectomy before age 45
? Low sex hormone levels in adults due to various causes
? Adults with a history of fragility fractures
? There are multiple risk factors for osteoporosis, such as old age, smoking, braking, long-term bed rest, etc
? People with a history of disease or use of drugs that affect bone metabolism
? Take the IOF Osteoporosis One-minute quiz, and if you answer "yes" to one of the questions, you are at potential risk for osteoporosis
? Postmenopausal women with OSTA index ≤-4 (OSTA index = [weight (kg) -age (years)] ×0.2)
What are the indicators of osteoporosis related laboratory tests?

1. General examination items: blood routine, urine routine, erythrocyte sedimentation rate, liver and kidney function, blood calcium, blood phosphorus, blood alkaline phosphatase, 25 hydroxyvitamin D (25OHD) and parathyroid hormone (PTH) levels, as well as urine calcium, urine phosphorus and urine creatinine, etc., to evaluate bone metabolic status.
2. Biochemical markers of bone turnover:
1) Bone formation markers: serum alkaline phosphatase (ALP), serum osteocalcin (N-MID), serum bone-derived alkaline phosphatase (B-ALP), serum type I procollagen C-terminal propeptide (P1CP), serum type I procollagen N-terminal propeptide (P1NP).
a) Alkaline phosphatase (ALP)
Physiological elevation of ALP is seen in children and pregnant women, pathological elevation is seen in liver and bile diseases, rickets, osteoporosis, hyperparathyroidism and so on.
b) Osteocalcin (N-MID)
Reflecting the specific indicators of bone formation, the increase indicates a relatively strong rate of bone synthesis in the body, which is seen in osteoporosis and hyperparathyroidism and other diseases, while the decrease indicates a slower rate of bone synthesis in the body, which may be related to calcium deficiency in the body. This test is mainly used to evaluate the efficacy of anti-bone reabsorption therapy (osteoporosis and hypercalcemia).
c) Serum bone-derived alkaline phosphatase (B-ALP)
B-ALP is derived from bone, can reflect the activity of bone, and is a specific marker of bone formation. Significantly elevated serum B-ALP is helpful for bone development and the diagnosis of orthopedic diseases in children, such as osteosis, osteoporosis, rickets, bone tumors, Paget's bone disease, etc.
d) Serum type I procollagen N-terminal propeptide (P1NP).
In the process of bone formation, type I procollagen is cleaved into amino terminal propeptide (P1NP), carboxyl terminal propeptide (P1CP) and type I collagen. As metabolites, P1NP and P1CP can sensitize the whole body bone formation status. However, because P1CP is metabolized quickly and is easily affected by hormone levels, P1NP can more accurately reflect osteoblast activity. It is mainly used to evaluate the efficacy of postmenopausal women with osteoporosis and Paget's bone disease.
2) Bone resorption markers: fasting 2-hour urinary calcium/creatinine ratio (Uca/Cr), serum tartrate-resistant acid phosphatase (TRACP), serum type I collagen cross-linked C-terminal peptide (CTX), etc.
a) Fasting 2h urinary calcium/creatinine ratio (Uca/Cr)
It reflects the excretion level of urinary calcium and indirectly reflects the function of bone metabolism. It can be used for diagnosis and therapeutic monitoring of primary osteoporosis and rickets.
b) Serum tartrate-resistant acid phosphatase (TRACP)
It is one of the isoenzymes of acid phosphatase and is a marker of bone resorption. Elevated levels are seen in primary hyperparathyroidism, chronic renal insufficiency, and high conversion osteoporosis.
c) Serum Type I collagen cross-linked C-terminal Peptide (CTX)
During bone resorption, type I collagen is broken down by osteoclasts, releasing amino-terminal peptide (NTx) and carboxy-terminal peptide (CTx). CTx contains α-CTx and its isomer β-CTx, both of which are structure-stable and will not be further degraded. Among them, β-CTx has been studied more as a sensitive and specific bone resorption marker. The test can be used to detect anti-bone reresorption therapy monitoring in postmenopausal women and individuals with osteopenia.
Among the above detection indicators, PINP and CTX are recommended in the Diagnosis and Treatment Guidelines for primary Osteoporosis (2022), which are markers reflecting the high sensitivity of bone formation and bone resorption, respectively. The specific functions of these two indicators include: assessing bone loss; Predicting fracture risk; Differential diagnosis of osteoporosis; Monitoring the therapeutic effect of osteoporosis.
Reference material
[1]Wang O, Hu Y, Gong S, et al. Osteoporos Int, 2015, 26:2631-2640.
[2] Chinese Society of Osteoporosis and Bone Mineral Salt Diseases. Chinese Journal of Osteoporosis and bone mineral salt Diseases, 2022, 15(06):573-611.
[3]Vasikaran S., Eastell R., Bruyere O, et al. Osteoporos Int, 2011, 22(2), 391-420.
[4] Chinese Society of Osteoporosis and Bone Mineral Salt Diseases. Chinese Journal of Endocrinology and Metabolism, 2021, 37(10):863-874.
[5]Gutierrez-Buey G et al. Clin Endocrinol (Oxf), 2019, 91(3): 391-399.
[6] Guidelines for the diagnosis and treatment of primary osteoporosis (2022). Chinese Journal of General Practice, 2023,26(17): 1671-1691. (in Chinese)
[7] Expert Consensus Committee on Osteoporosis Diagnosis and Treatment in Primary Medical Institutions of China Health Promotion Foundation. Chinese Journal of Osteoporosis, 2021, 27(7): 937-944.
[8]Leder et al. J Clin Endocrinol Metab, 2014, 99(5): 1694-1700.


